Dental Implant Procedure Step by Step: A Comprehensive Guide

Dental implants have become a popular and effective solution for replacing missing teeth, providing a strong foundation for fixed or removable replacement teeth. This comprehensive guide will take you through the dental implant procedure step by step, ensuring you understand each stage of the process, from initial consultation to final restoration.

- Introduction to Dental Implants
- Initial Consultation and Examination
- Treatment Planning
- Preparatory Procedures
- Bone Grafting
- Sinus Lift
- Implant Placement Surgery
- Anesthesia Options
- Implant Insertion
- Osseointegration Period
- Abutment Placement
- Final Restoration
- Impressions and Models
- Crown Fabrication
- Post-Procedure Care and Maintenance
- Potential Risks and Complications
- Benefits of Dental Implants
- Cost Considerations and Insurance
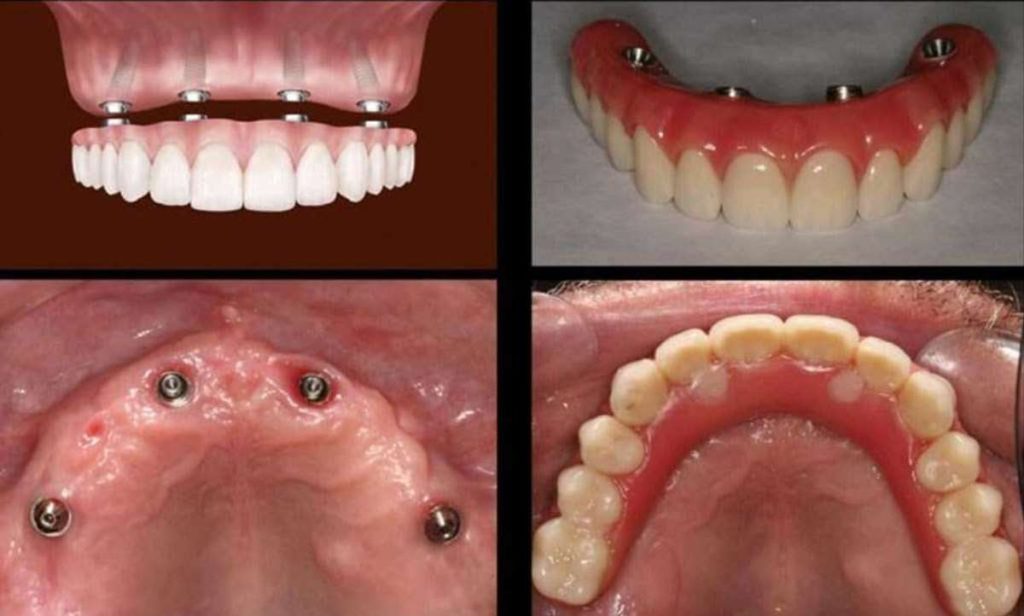
1. Introduction to Dental Implants
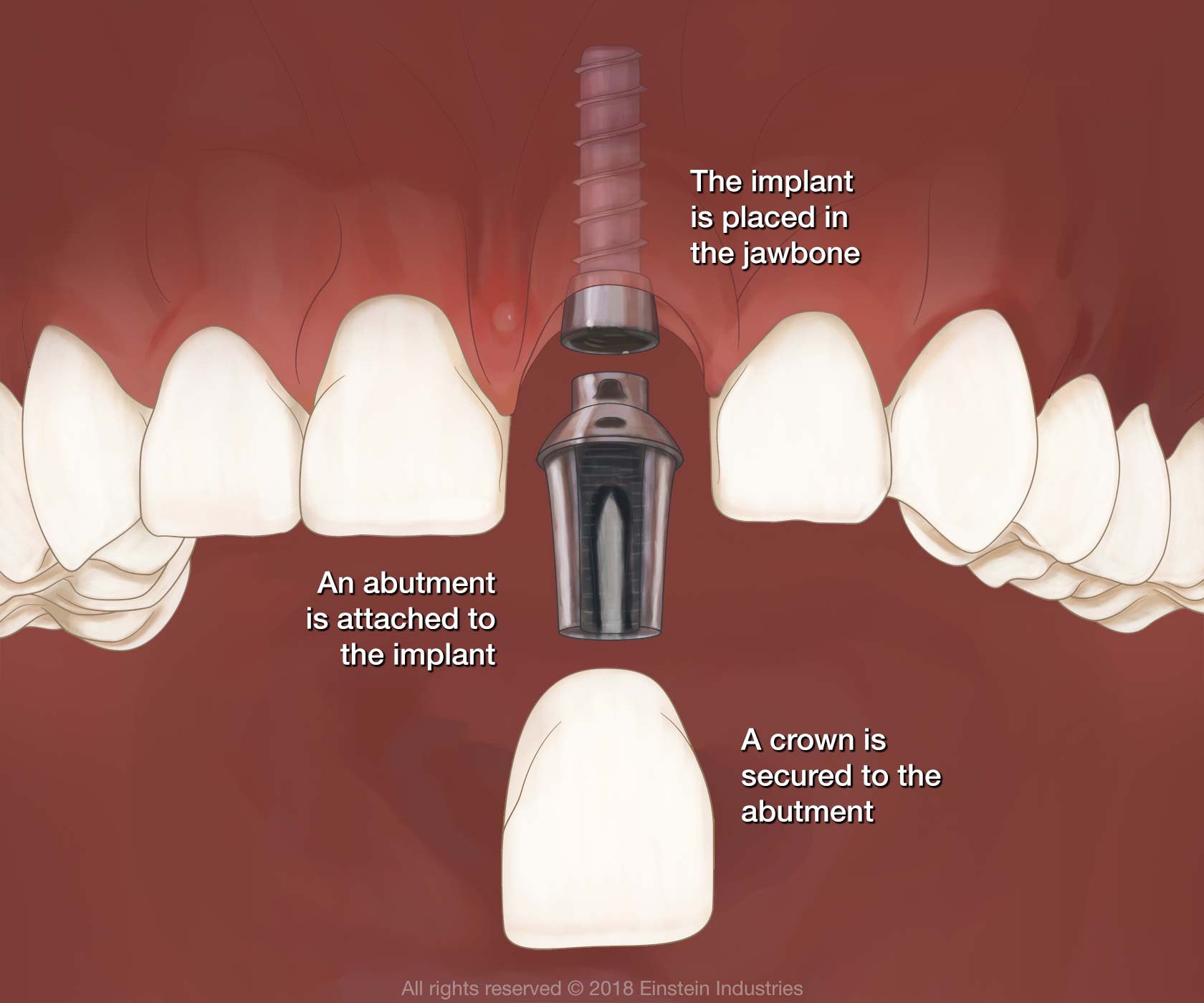
Dental implants are artificial tooth roots made of biocompatible materials, usually titanium, that are surgically placed into the jawbone. They serve as a sturdy base for attaching replacement teeth, such as crowns, bridges, or dentures. Dental implants mimic the look and function of natural teeth, offering a permanent solution for tooth loss.
2. Initial Consultation and Examination
The first step in the dental implant procedure is a thorough consultation and examination with a dental professional. During this visit, the dentist will:
- Review your medical and dental history
- Conduct a comprehensive oral examination
- Take dental X-rays and 3D scans to assess bone structure and oral health
- Discuss your treatment goals and expectations
This initial consultation is crucial for determining if you are a suitable candidate for dental implants.
3. Treatment Planning
Based on the information gathered during the initial consultation, the dentist will develop a personalized treatment plan. This plan outlines the entire process, including:
- The number of implants needed
- The type of implant system to be used
- Any preparatory procedures required, such as bone grafting or sinus lift
- The timeline for each phase of the procedure
The treatment plan is tailored to your specific needs and ensures a successful outcome.
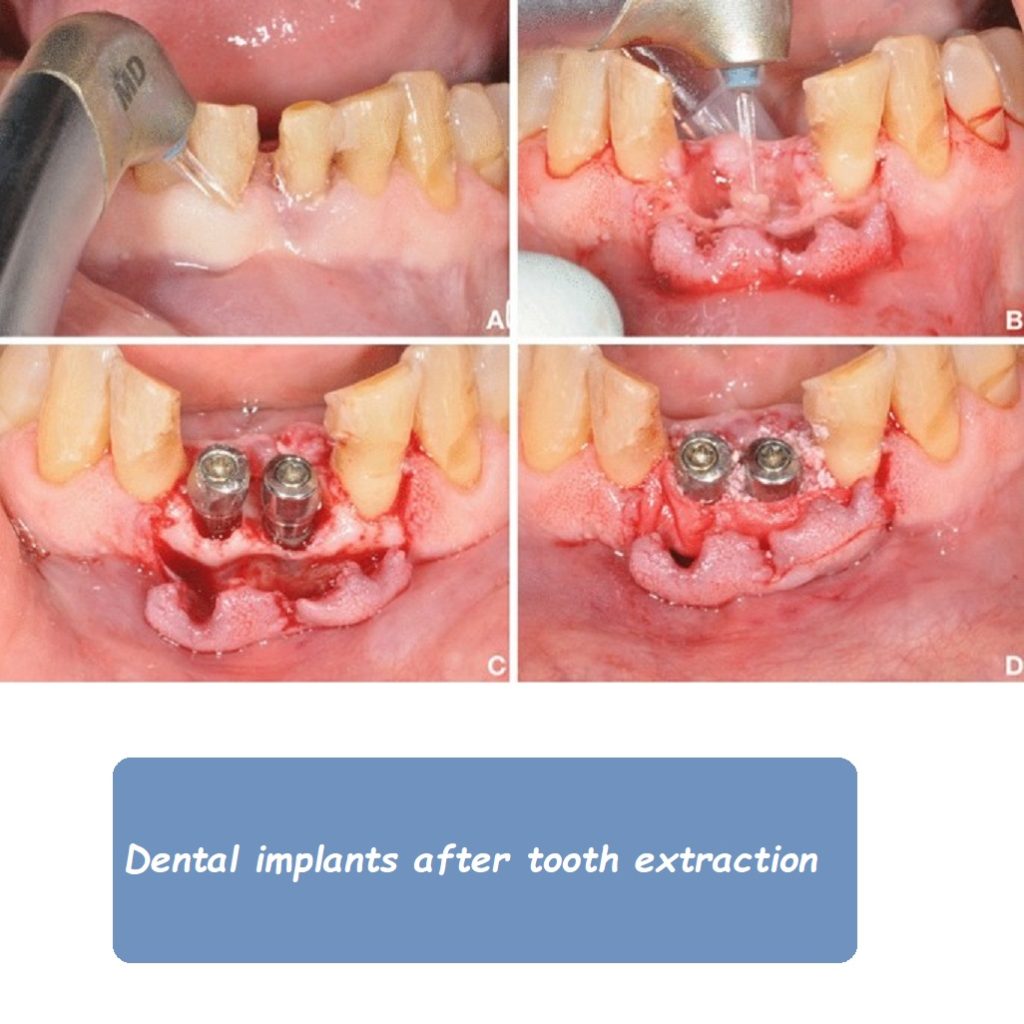
4. Preparatory Procedures
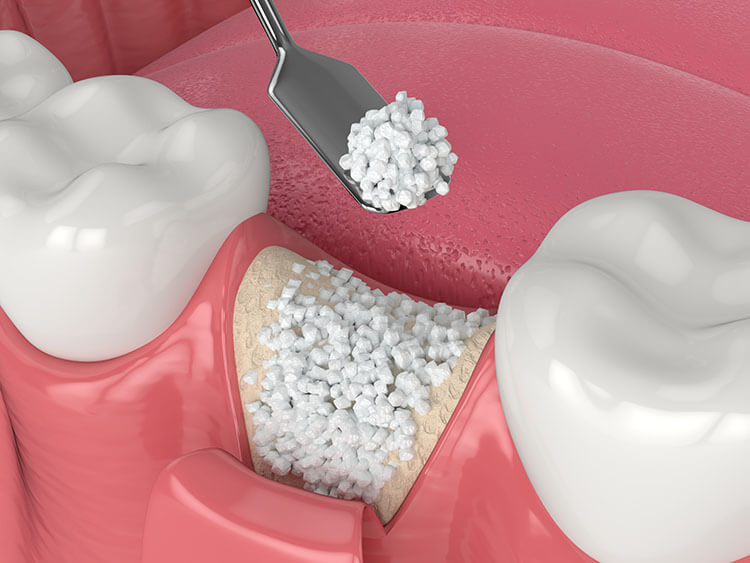
Bone Grafting
In some cases, patients may not have sufficient bone density in the jaw to support dental implants. Bone grafting is a procedure that involves adding bone material to the implant site to enhance bone volume and density. There are different types of bone grafts:
- Autograft: Bone taken from another part of the patient’s body
- Allograft: Bone from a human donor
- Xenograft: Bone from an animal source
- Synthetic graft: Artificial bone material
The bone grafting procedure is performed under local anesthesia, and the graft material is placed in the deficient area. The healing period for bone grafting can range from several weeks to a few months.
Sinus Lift
For patients requiring implants in the upper jaw, a sinus lift may be necessary if there is insufficient bone height. The sinus lift procedure involves lifting the sinus membrane and adding bone graft material to create a stable foundation for the implant. This procedure is typically performed by an oral surgeon and requires a healing period of several months before implant placement.
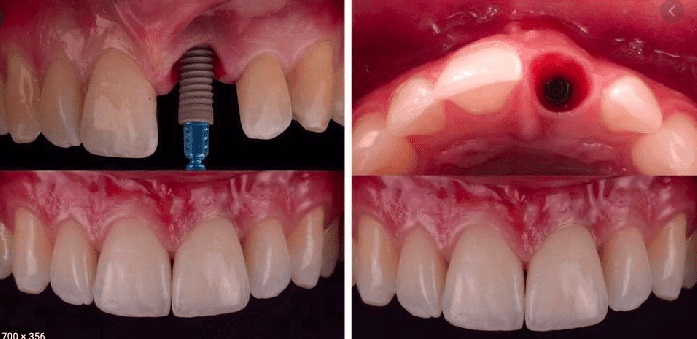
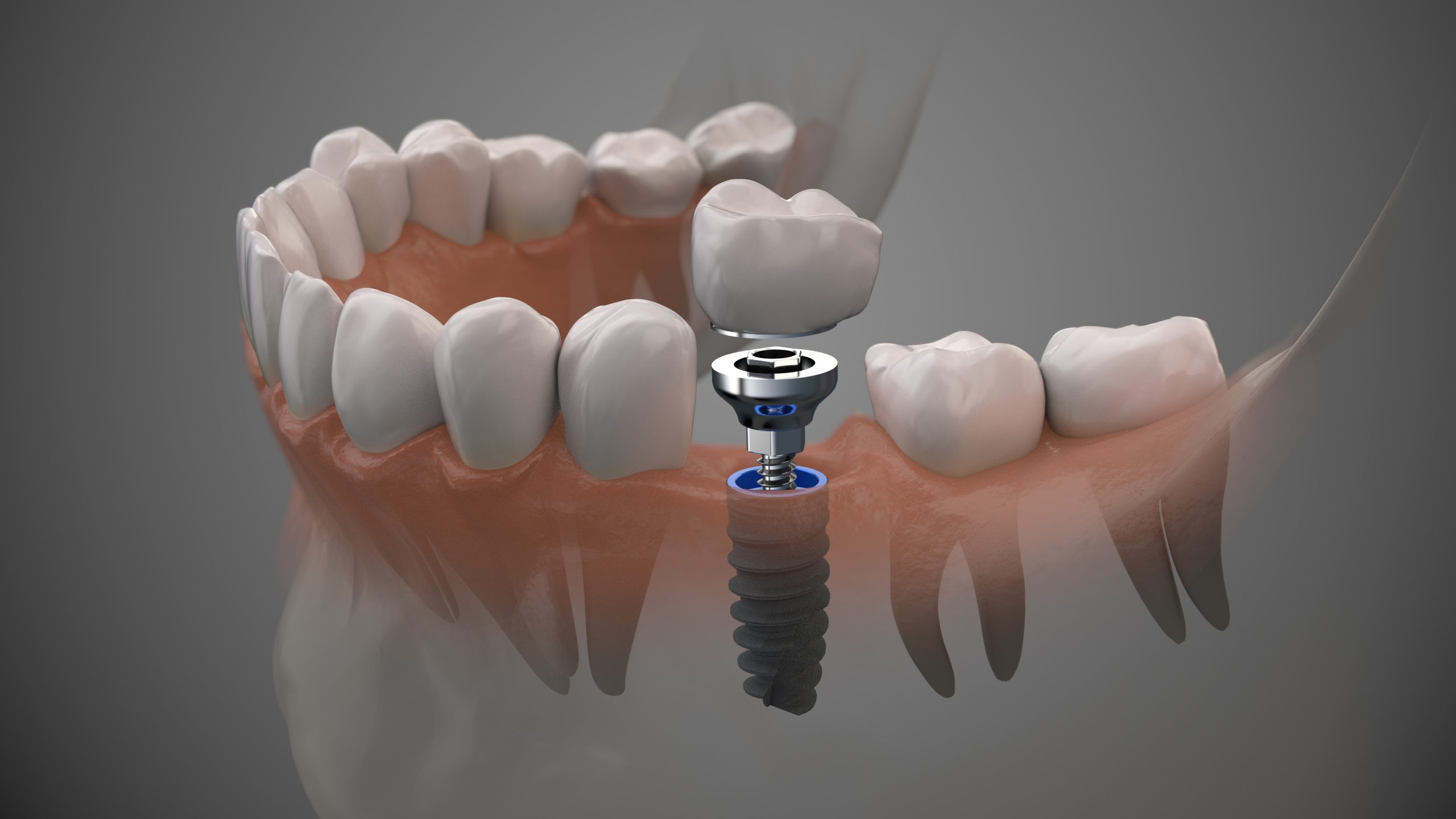
5. Implant Placement Surgery
Anesthesia Options
Dental implant surgery is usually performed under local anesthesia, but sedation options are available for patients with dental anxiety. The anesthesia ensures a pain-free experience during the procedure.

Implant Insertion
The implant placement surgery involves the following steps:
- Incision: The dentist makes a small incision in the gum tissue to expose the jawbone.
- Drilling: A series of progressively larger drills are used to create a hole in the bone for the implant.
- Implant Placement: The titanium implant is inserted into the prepared hole.
- Suturing: The gum tissue is stitched back into place to cover the implant.
This surgical procedure usually takes about 1-2 hours per implant, and patients can go home the same day.
6. Osseointegration Period
After the implant is placed, a critical process called osseointegration begins. Osseointegration is the natural fusion of the implant with the jawbone, providing a stable and durable foundation for the replacement tooth. This process can take 3-6 months, during which the patient must follow specific care instructions to ensure successful healing.

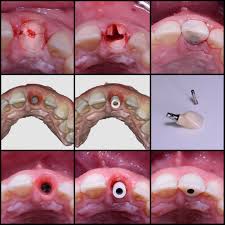
7. Abutment Placement
Once osseointegration is complete, a second minor surgery is performed to attach an abutment to the implant. The abutment serves as a connector between the implant and the replacement tooth. The steps involved in abutment placement are:
- Incision: A small incision is made in the gum tissue to expose the implant.
- Abutment Attachment: The abutment is screwed onto the implant.
- Suturing: The gum tissue is closed around, but not over, the abutment.
The gum tissue will heal around the abutment over a couple of weeks, creating a natural appearance.
8. Final Restoration
Impressions and Models
With the abutment in place, the dentist will take impressions of your mouth to create accurate models for the final restoration. These impressions are used to design custom-made replacement teeth that fit seamlessly with your natural teeth.
Crown Fabrication
The final restoration, typically a crown, is fabricated in a dental laboratory using the impressions. Crowns can be made from various materials, including porcelain, ceramic, or metal. The choice of material depends on factors such as aesthetics, strength, and patient preference.
Once the crown is ready, it is securely attached to the abutment, completing the dental implant procedure. The final restoration is designed to blend in with your natural teeth, providing a functional and aesthetically pleasing result.
9. Post-Procedure Care and Maintenance
Proper care and maintenance are essential for the long-term success of dental implants. Patients should follow these guidelines:
- Practice good oral hygiene, including brushing and flossing
- Attend regular dental check-ups and cleanings
- Avoid hard or sticky foods that can damage the implants
- Use a mouthguard if you grind your teeth
Following these recommendations helps ensure the longevity and health of your dental implants.
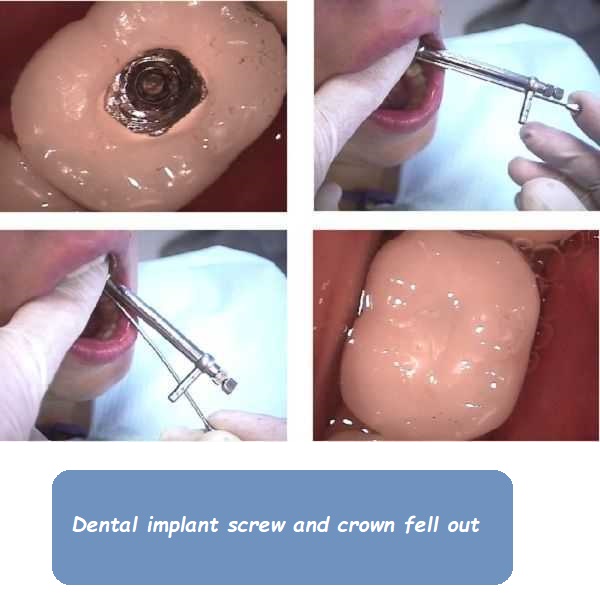
10. Potential Risks and Complications
While dental implants have a high success rate, there are potential risks and complications to be aware of:
- Infection: Infection at the implant site can occur if proper oral hygiene is not maintained.
- Implant Failure: In rare cases, the implant may not integrate with the bone, leading to failure.
- Nerve Damage: Implant placement near nerves can cause numbness or tingling in the lips, tongue, or chin.
- Sinus Issues: Implants placed in the upper jaw can protrude into the sinus cavities, causing sinus problems.
Patients should discuss these risks with their dentist and follow all care instructions to minimize complications.
11. Benefits of Dental Implants
Dental implants offer numerous benefits over other tooth replacement options:
- Durability: Implants are designed to last a lifetime with proper care.
- Aesthetics: Implants look and feel like natural teeth.
- Functionality: Implants restore full chewing and speaking abilities.
- Bone Preservation: Implants stimulate the jawbone, preventing bone loss.
These benefits make dental implants a preferred choice for many patients seeking tooth replacement solutions.
12. Cost Considerations and Insurance
The cost of dental implants can vary depending on factors such as the number of implants needed, the complexity of the case, and geographic location. On average, a single dental implant can cost between $3,000 and $5,000. This price includes the implant, abutment, and crown.
While dental insurance plans may cover a portion of the cost, patients should check with their insurance provider to understand their coverage. Some dental offices also offer financing options to help make the procedure more affordable.
Conclusion
Dental implants are a highly effective solution for replacing missing teeth, offering a durable and natural-looking result. Understanding the dental implant procedure step by step helps patients make informed decisions and prepares them for each stage of the process. From the initial consultation to the final restoration, dental implants provide a permanent solution that can significantly improve oral health and quality of life. By following proper care and maintenance guidelines, patients can enjoy the benefits of dental implants for many years to come.
Related to read:
Best Oral Hygiene Practices For Optimum Oral Health.
How to Whiten Teeth Naturally?
How to keep your gums healthy and disease-free?
References
To ensure the information provided is accurate and up-to-date, the following sources were referenced:
- American Dental Association. (n.d.). Plaque and Tartar. Retrieved from ADA website
- Mayo Clinic. (n.d.). Dental Plaque. Retrieved from Mayo Clinic website
- National Institute of Dental and Craniofacial Research. (n.d.). Periodontal (Gum) Disease. Retrieved from NIDCR website